Unveiled connection: Vitamin D could influence birth control effectiveness
A Fresh Take on the Impact of Birth Control on Vitamin D Levels
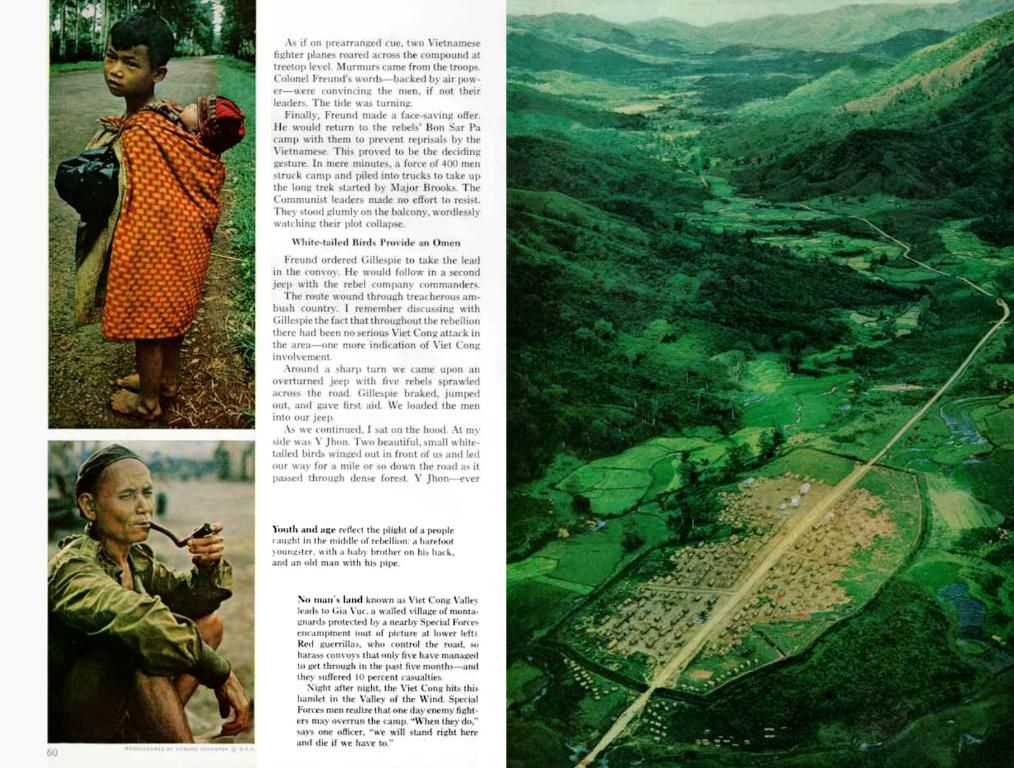
Vitamin D, often known as the sunshine vitamin, plays a crucial role in maintaining healthy calcium and phosphorous levels in the blood, and aiding the body's absorption of calcium, a vital component of bones. With various food sources, including fish and eggs, and around 90% produced through a chemical reaction in the skin after sun exposure, vitamin D deficiency can lead to bone issues like rickets and osteomalacia.
During pregnancy, the role of vitamin D becomes even more significant due to the increased need to support the growth of the fetal skeleton. This makes pregnant women more prone to vitamin D deficiency and related health problems.
Such insights prompted Dr. Quaker E. Harmon of the National Institutes of Health's National Institute of Environmental Health Sciences to delve into the association between vitamin D levels and oral contraceptives containing estrogen.
Vitamin D and Contraception: Unraveling the Connection
Intrigued by the potential link, Harmon and her team conducted a cross-sectional analysis of data from the Study of Environment, Lifestyle, and Fibroids (SELF), which focused on reproductive health. By asking participants about their contraceptive use, sunlight exposure, and vitamin D supplementation, they gathered data from 1,662 African-American women aged 23-34.
Blood samples were analyzed to measure levels of the most common circulating form of vitamin D – 25-hydroxy vitamin D. The study found that women using contraception containing estrogen had significantly higher vitamin D levels. Their findings remained statistically significant even after accounting for confounding factors like exposure to light.
The study further discovered that current users of birth control had higher levels of vitamin D, while past users had average levels. This association persisted, suggesting that contraceptives containing estrogen may boost vitamin D levels, and these levels may drop after women stop using contraception.
After adjusting for confounding variables, the use of contraceptive pills, patches, or rings containing estrogen was linked to a 20% increase in 25-hydroxy vitamin D levels.
Vitamin D Deficiency in Early Pregnancy
The findings, published in the Journal of Clinical Endocrinology & Metabolism, shed light on the potential risks women face when trying to conceive. In Dr. Harmon's words, "[A] woman starting to try to become pregnant runs the risk of becoming deficient in vitamin D."
She recommends that women planning to cease using birth control take precautions to ensure adequate vitamin D levels while trying to conceive and during pregnancy. However, more research is needed to understand the mechanisms behind the observed association and how it differs across various racial groups.
The current study focused solely on African-American women; it remains unclear if race might play a role in this effect. Dr. Harmon explains, "The same association has been observed in women who are not African-American, so we believe this association is not related to race."
Harmon is currently following this cohort to further investigate the relationship and studying another group of participants to explore how vitamin D levels vary across the menstrual cycle.
While the exact reasons behind the relationship between estrogen-based contraception and vitamin D levels remain unknown, insights into hormonal influence on calcium metabolism suggest possible indirect effects. Further research is essential to fully grasp the intricacies of this interaction and how it may impact different racial groups.
- The study published in the Journal of Clinical Endocrinology & Metabolism found that women using contraception containing estrogen had significantly higher vitamin D levels, indicating a potential link between the two.
- In light of this discovery, Dr. Harmon advises women planning to cease using birth control to ensure adequate vitamin D levels while trying to conceive and during pregnancy.
- The findings suggest that contraceptives containing estrogen may boost vitamin D levels, and these levels may drop after women stop using contraception.
- The study, which focused on African-American women, discovered that current users of birth control had higher levels of vitamin D, while past users had average levels.
- The association between estrogen-based contraception and vitamin D levels persisted, implying a need for further research to understand the mechanisms behind it and how it might differ across various racial groups.
- The current study serves as a stepping stone for future research, with Dr. Harmon continuing to investigate the relationship and studying another group of participants to explore how vitamin D levels vary across the menstrual cycle, aiming to fully grasp the intricacies of this interaction and its potential impact on women's health and nutrition.